By: Kyrié Carpenter
 Do you have a family member who is bright and doing a good job managing their day-to-day, but seem to forget things like, “Did I eat breakfast today?” or “What is your name?” If this sounds like your loved one, it’s possible that he or she may be experiencing what is called MCI (Mild Cognitive Impairment).
Do you have a family member who is bright and doing a good job managing their day-to-day, but seem to forget things like, “Did I eat breakfast today?” or “What is your name?” If this sounds like your loved one, it’s possible that he or she may be experiencing what is called MCI (Mild Cognitive Impairment).
If you couldn’t find your car keys this morning, do not panic. As ageism activist Ashton Applewhite says, “When we lost our car keys as teenagers, we did not call it a junior moment.” All of us, at every age, have forgetful moments.
Globally, only 6% of people in their 60s have MCI. By 85 that number only rises to 37%. Mild Cognitive Impairment is not dementia and will not necessarily progress into it. Early stages of dementia can manifest similarly to MCI. It is important to be aware of memory changes in yourself or a loved one so that you make helpful changes in your lifestyle.
The Two Types of Mild Cognitive Impairment
Medical professionals have identified two types of Mild Cognitive Impairment:
- Amnestic MCI. This form of MCI primarily affects memory. Your loved one may be forgetting appointments, conversations or recent events more often.
- Nonamnestic MCI. This form of MCI primarily affects thinking skills other than memory. Your loved one may have trouble judging the time or sequence of steps needed to complete a complex task or visual perception.
As with dementia, it is important to note that MCI is not a ‘disease’ in the traditional sense. There is no virus, bacteria or direct cause we can use to identify or fight it.
What are the Signs of MCI?
Mild Cognitive Impairment is diagnosed by a neurologist, memory clinic or neuropsychologist. A diagnosis of MCI does not mean you will have progressive dementia such as Alzheimer’s disease. About fifty percent of those with MCI are later diagnosed with dementia. This is likely because of the early stages of dementia present as MCI. The other fifty percent never progress further than this challenge with memory. The signs of MCI include:
- Misplacing things often
- Forgetting to go to events or appointments
- Having more trouble coming up with words than other people of the same age
A medical workup for MCI includes the following core elements:
- A thorough review of one’s medical history
- An assessment of independent function and daily activities. This focuses on any changes from a person’s usual level of function. Input from a family member or trusted friend is often used to provide an additional perspective.
- An assessment of mental status. Brief tests measuring memory, planning, judgment and other key thinking skills are administered.
- In-office neurological exams of nerves and reflexes, movement, coordination, balance and senses.
- Evaluations of mood to detect depression. Symptoms may include problems with memory or feeling “foggy.”
- Laboratory tests including blood tests and imaging of the brain’s structure
If the above is inconclusive, neuropsychological tests may be ordered.
What are the Risk Factors for MCI?
There are modifiable risk factors that increase the severity of MCI and dementia. According to Dr. Kristine Yaffee at UCSF’s Memory Center they include:
- Type 2 diabetes
- High blood pressure
- Midlife obesity
- Smoking
- Depression
- Little or no mental activity
- Little or no physical exercise
If any of these apply to you, talk to your doctor about how to modify them!
10 Ways to Reduce Your Risk of MCI and Live a Better Life with MCI
Even if you receive a diagnosis of MCI, or dementia for that matter, that is not the end of the story. There are many things you can do to improve your quality of life and optimize your cognitive function.
Currently, there are no approved medications for the treatment of MCI. Below is a list of things you can do that have been shown to improve cognitive function and quality of life.
- Check for treatable causes. Things such as sleep deprivation and other health conditions can cause cognitive decline. If these are treated, often the cognitive ability will return. Loss of hearing and changes in eyesight can also mimic cognitive decline. Have regular medical check-ups. Be sure to check your hearing and eyesight annually as well
- Learn a new skill. Learning something new engages your brain in new and different ways. You can jumpstart it into making new pathways to find information and function.
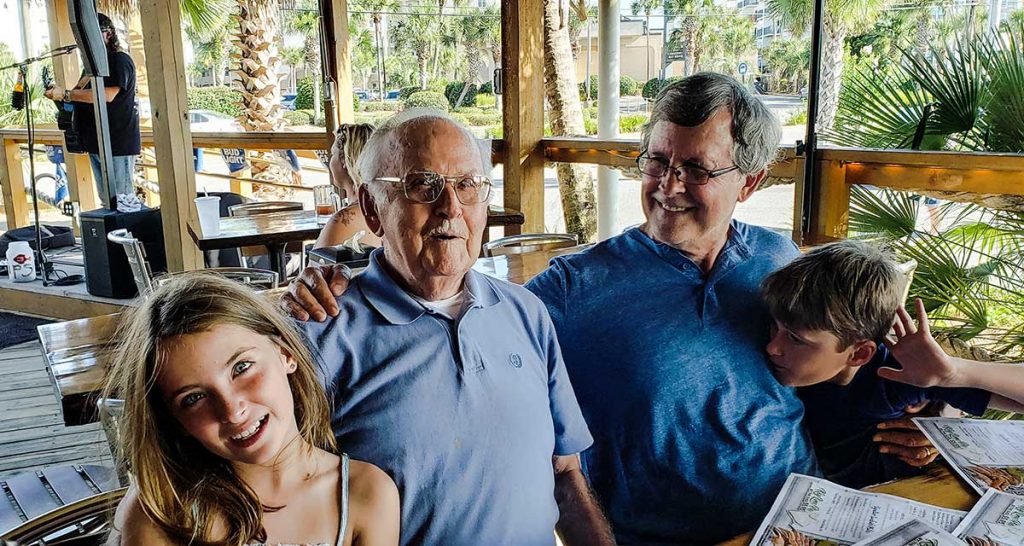
- Build community. Be engaged in social activities daily. Try playing cards, joining a book club, or spending time with friends and family. Do what is meaningful to you.
- Volunteer. You can do this in your community, at a school, or at your place of worship.
- Use support. Use memory tools such as calendars, to-do lists, and notes to yourself. New technology is constantly emerging to function as cognitive prosthetics. There should be no shame in using technology for support. Think of phone numbers; there was a time when we all memorized them. Now, it is commonplace to use a ‘cognitive prosthetic’ of the contacts saved in our phone to recall numbers.
- Form habits. Put your wallet or purse, keys, glasses and other daily use objects in the same place each day.
- Get lots of rest. As we age sleep comes in smaller more spread out packages. This is called sleep fragmentation and is totally okay. Listen to your body and get the right amount of rest in the right ways for you. Say yes naps!
- Exercise. Try to do aerobic exercise two to three times a week for 30 minutes. Bonus points if you fit in some strength building and balance work too! According to findings compiled by Harvard, “Exercising can offer mental and social stimulation while improving blood flow to the brain, possibly even prompting the release of molecules that repair brain cells and create connections between them.” Exercise can help keep blood pressure in check. Emerging research presented by the Alzheimer’s Association showed a 19% reduction in MCI for those who received intensive blood pressure treatment.
- Eat well. Forget about fad diets. The best advice about eating comes from Michael Pollan who says to eat a variety of foods, not too much and mostly plants.
- Get help if you feel depressed. Living with cognitive change can come with a lot of prejudice and shame. Get support in dementia inclusive spaces.
The bottom line: If you or someone you love is experiencing cognitive change don’t panic. There is a lot you can do to help increase brain function and quality of life.
Resources
Staving Off Dementia When You Have Mild Cognitive Impairment
What is Mild Cognitive Impairment
Noticing Memory Problems? What To Do Next.
Exercise and Physical Activity: Getting Fit for Life
Sprint for Discovery: New Dementia and Cardiovascular Findings





